Paediatric palliative care: a parent’s perspective
By Renee Swannack
Palliative care. The words conjure up thoughts of terminal illness, emergency meetings, heartbreaking goodbyes, desperately clinging to whatever time is left with loved ones.
They’re not words anyone would ever wish to be associated with a child.
Our son was 3 months old when his neurologist gently explained that his condition was life limiting. He gave us a heart wrenching time frame of life expectancy for children with similar devastating forms of epilepsy. It’s a wide frame, but the crushing fact that we’ll say goodbye to our child remains.
For a long time I avoided opening up about my feelings, as if discussing it would jinx my son. As if speaking out loud about it would cause it to happen sooner than it should. I also found it difficult to even find the words I needed to express the unbearable pain I felt and still feel.
The heart-broken feeling of anticipatory grief. The cruel reality of our situation is that things can take a turn for the worst at any time; we’re constantly fighting to keep this at bay. Every dose of medication, every suction of secretions in his airways, every time he’s treated for a chest infection. Every new cluster of seizures the medications don’t control.
Every night when we turn on his seizure monitor after we’ve snuggled him to sleep.
I try not to think about it, but fear creeps in at obvious times, like ambulance rides and when we’re being met-called into ICU. The toughest is when it crosses my mind during good times.
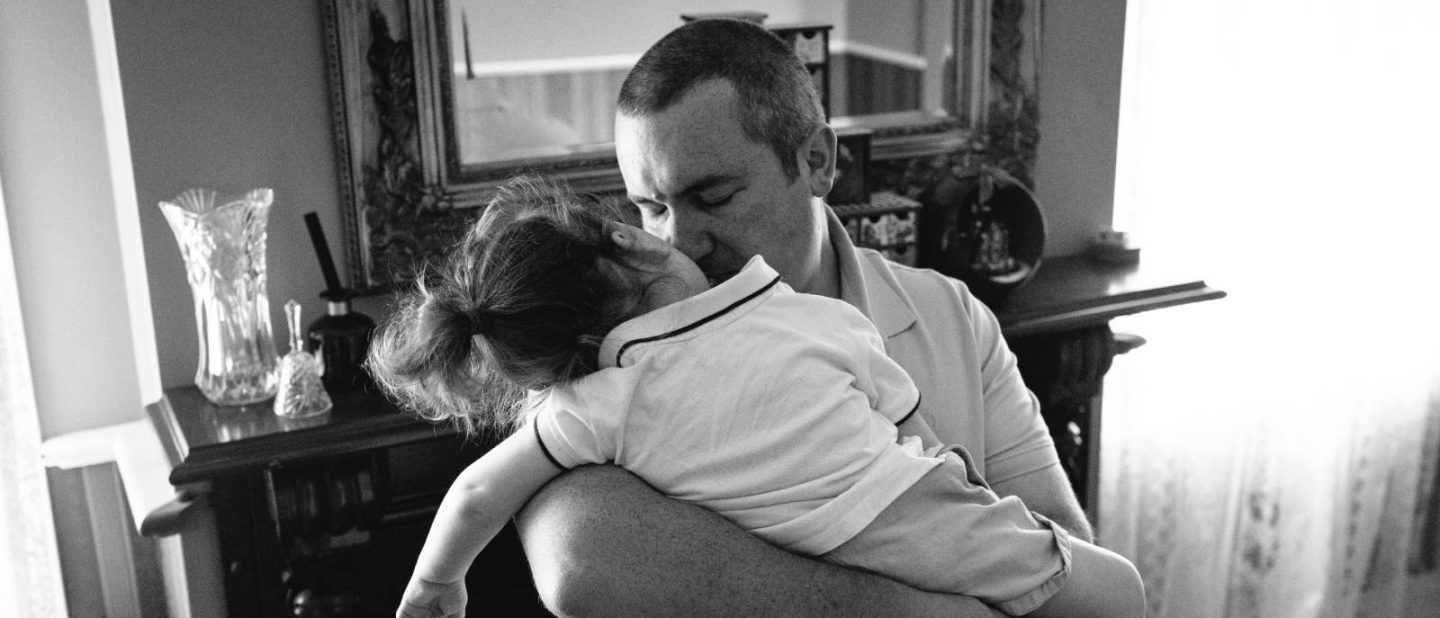
Thankfully, our son lives his life full of joy. It’s difficult not to match his love of life. With each smile and giggle he reminds us to stop and enjoy the moment. To move through our fears and create as many beautiful moments together as we possibly can.
After a particularly close call that we certainly weren’t prepared for, a friend of mine who had recently said goodbye to her own beautifully complex son, gently suggested that we request our son be under the care of our hospital palliative care team.
Naturally, I reeled at the idea. The thought of him being cared for by a palliative care team would shine a light on the harsh reality of our situation. My friend reassured me that palliative care looks very different for children than it does for adults, that it’s more about being prepared and supported than anything else. I parked the idea in the back of my mind, but also knew that children like mine need a specific type of care, as do their families.
I turned to the internet for a little more information and again felt reassured by what I found. ‘Palliative care for children and young people with life-limiting conditions is an active and total approach to care, embracing physical, emotional, social and spiritual elements. It focuses on enhancement of quality of life for the child and support for the family and includes the management of distressing symptoms, provision of respite, and care through death and bereavement.
After opening up to our son’s paediatrician about my feelings, she referred us to the RCH Palliative Care team. The introduction and first few conversations were emotional, but there was a sense of ‘hoping for the best but preparing for the worst’ which I appreciated. We discussed our definitions of quality of life, of comfort and end of life care, which medical interventions we were comfortable with and how we would appreciate their expertise and guidance when it came to making such huge decisions. They also reassured us that nothing is ever set in stone and that different situations may require different decisions and that all of this is perfectly fine.
We now know we have a team around us that understands our hopes, dreams and fears. A team who can answer the tough questions, help us to navigate the medical system, can work alongside and support other teams who also provide care, ensuring our sons needs are being met and that we feel supported.
They’re familiar faces during hospital admissions, a phone call when things are quiet to ensure we’re all okay and a bonus in that they tend to have a fantastic sense of humour, not an easy task to master in such a serious setting, but they do it well.
Most importantly they genuinely care for our son and appreciate the happy, loving, sweet little boy that he is.
Knowing that when the time comes, they will be there to support us through our toughest days brings a comfort we wish we didn’t need, but one we’re grateful to have.
By helping carry some of the weight of our situation, our son’s palliative care team leave more time for us to spend loving him.
Which is the one thing we need most of all.
Renee is Co-Founder of ‘How to Make Lemonade’ – a platform created by three mums who share their musings about life raising children with complex medical conditions and additional needs. Celebrating the good, the bad, the downright ridiculous, and doing whatever they can to have a laugh along the way. facebook.com/lemonadevillage







