
Understanding dysphagia in children and young people with disability
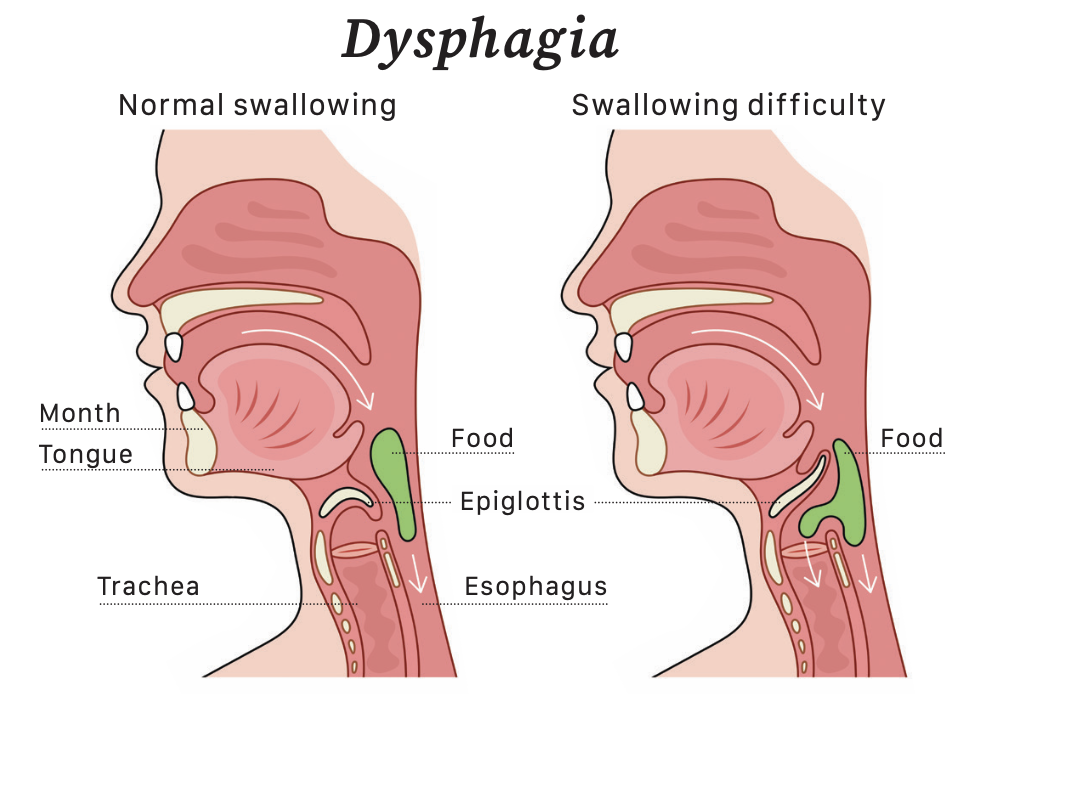
Swallowing is a reflex action that is easy to take for granted, but it can be complicated and challenging, especially for those with dysphagia. The process of swallowing involves a coordinated effort of muscles and nerves, ensuring that food and liquids move safely from the mouth to the stomach. When this process is disrupted, it can lead to various complications, especially in someone who already faces challenges due to their diagnosis. Here’s what you need to know if your child or young person is affected.
TYPES OF DYSPHAGIA
Dysphagia in children can be classified into two main types: oropharyngeal dysphagia and oesophageal dysphagia.
Oropharyngeal Dysphagia
Chewing difficulty: Children may struggle with chewing food thoroughly, leading to problems with bolus formation (food mass) for swallowing.
Oral sensory issues: Some children may have hypersensitivity or hyposensitivity in their oral cavity, affecting their ability to manage different food textures.
Swallowing coordination: Challenges in coordinating the muscles involved in swallowing, including the tongue, soft palate, and pharynx, can cause food or liquids to enter the airway instead of the oesophagus.
Oesophageal Dysphagia
Oesophageal motility disorders:
Conditions such as achalasia or oesophageal strictures can result in difficulties in food passage through the oesophagus.
Structural abnormalities: Anatomical abnormalities in the oesophagus, such as webs, rings, or narrowing, can impede the smooth flow of food.
Gastroesophageal reflux disease (GERD): People with disability may be more prone to GERD, leading to oesophageal irritation and discomfort during swallowing.
Causes and associated diagnoses
Dysphagia in people with disability can arise from various underlying conditions, including cerebral palsy, Down syndrome, muscular dystrophy, and neurological disorders. These conditions can affect muscle tone, coordination, and sensory responses involved in the swallowing process. For example, people with cerebral palsy may experience spasticity or weakness in the muscles used for swallowing, while those with Down syndrome may have anatomical differences in their oral structures that impact swallowing.
IDENTIFYING DYSPHAGIA
Identifying dysphagia in children with disabilities requires careful observation and monitoring. It is crucial to consult with healthcare professionals, including a paediatrician and a speech-language pathologist if you suspect there is an issue; they can conduct a thorough evaluation and recommend appropriate interventions. Here are some common symptoms to watch for:
PHYSICAL SIGNS AND SYMPTOMS
Coughing or choking during meals
Frequent coughing or choking while eating or drinking is one of the most noticeable signs of dysphagia. It indicates that food or liquid may be entering the airway instead of the oesophagus.
Gagging or spitting out food
People with dysphagia may gag or spit out food frequently. This can happen because they are unable to chew and swallow effectively.
Drooling or excessive saliva
Persistent drooling or an inability to manage saliva can be a sign of swallowing difficulties. This is particularly noticeable when a child is not teething.
Wet or gurgly voice
A wet or gurgly sounding voice during or after eating or drinking can indicate that food or liquid is not being swallowed properly and may be lingering in the throat.
Recurrent respiratory infections
Frequent respiratory infections, such as pneumonia or bronchitis, can occur if food or liquids are aspirated (enter the airway), leading to infection in the lungs.
BEHAVIOURAL SIGNS
Reluctance to eat certain foods Children with dysphagia may develop aversions to specific food textures or consistencies, leading to picky eating or refusal to eat.
Extended mealtime duration
Taking an unusually long time to eat meals can be a sign that the child is struggling with the process of chewing and swallowing.
Avoidance of solid foods
Preference for liquids or very soft foods over solids can indicate difficulty in managing more complex textures during swallowing.
Behavioural changes at mealtime
Increased fussiness, irritability, or anxiety during meals can be related to the discomfort or frustration associated with swallowing difficulties.
NUTRITIONAL AND GROWTH CONCERNS
Poor weight gain or weight loss Inadequate nutrition due to swallowing difficulties can lead to poor weight gain or even weight loss. Monitoring growth patterns is essential.
Dehydration
If someone has dysphagia they may struggle to drink enough fluids, leading to signs of dehydration such as dry mouth, decreased urination, and lethargy.
Malnutrition
Difficulty swallowing can result in an imbalanced diet and nutrient deficiencies. Signs of malnutrition include fatigue, weakness, and poor overall health.
ASSESSMENT AND MANAGEMENT
Early detection and intervention are crucial in managing dysphagia.
A comprehensive assessment by a multidisciplinary team, including speech- language pathologists, paediatricians, gastroenterologists, and dietitians, is essential. This assessment may involve clinical evaluations, swallowing studies (such as videofluoroscopic swallow study or fibre-optic endoscopic evaluation), and nutritional assessments to understandthe nature and severity of the swallowing difficulties.
Management strategies are tailored to each individual’s needs but may include:
Diet modification: Adjusting the consistency and texture of foods and liquids to ensure safe swallowing. Thickening liquids or pureeing foods can make them easier to swallow for some children.
Positioning techniques: Optimal positioning during meals, such as sitting upright or at a specific angle, can improve swallowing function and reduce the risk of aspiration.
Swallowing therapy: Working with a speech-language pathologist to perform exercises and techniques aimed at strengthening swallowing muscles, improving coordination, and addressing sensory issues related to feeding.
Medical interventions: In some cases, medical interventions such as botulinum toxin injections to reduce muscle spasticity, gastrostomy tube placement for nutritional support, or surgical procedures to correct anatomical abnormalities may be considered.
Support and education
Parents, caregivers, and educators play a vital role in supporting children with dysphagia. They should receive education and training on proper feeding techniques, recognising signs of swallowing difficulties, and implementing strategies recommended by healthcare professionals. Creating a supportive and nurturing mealtime environment is essential for promoting positive feeding experiences and ensuring the child’s nutritional needs are met.
MANAGING DYSPHAGIA AT SCHOOL
Coping with dysphagia at school requires careful planning, collaboration between the child, parents, school staff, and healthcare professionals, and implementation of risk management strategies to ensure the child’s safety and well-being. Here’s how a child with dysphagia might cope at school and the risk management strategies that might need to be in place:
1.Care plan
Develop an individualised care plan in collaboration with the child’s healthcare team, outlining specific dietary needs, feeding techniques, positioning requirements,
and any medical interventions or emergency protocols.
Communicate the plan to relevant school personnel, including teachers, school nurses, cafeteria staff, and administrators, to ensure everyone is aware of the child’s needs and how to support them.
2. Education and training
Provide education and training to school staff on dysphagia awareness, signs of swallowing difficulties, and proper implementation of feeding protocols.
3. Safe feeding environment
Create a safe and supportive feeding environment in designated eating areas. Ensure that tables and chairs are appropriately sized, seating is comfortable and stable, and distractions are minimised during mealtimes.
Encourage the child to eat slowly, take small bites, and chew thoroughly to reduce the risk of choking or aspiration. Provide adaptive utensils, straws, or cups if needed.
4. Mealtime supervision
Assign trained staff members to supervise the child during meals and snacks, monitoring their eating behaviour, swallowing function, and signs of distress.
Encourage peer support and understanding among classmates to promote inclusivity and reduce social stigma related to feeding difficulties.
5. Communication and advocacy
Foster open communication between parents, school staff, and healthcare providers to address any concerns, monitor progress, and adjust management strategies as needed.
Empower the child to advocate for themselves by teaching them communication strategies to
express their needs, preferences, and any discomfort related to dysphagia.
6. Emergency preparedness
Develop an emergency action plan detailing steps to take in case of a choking incident, aspiration event, or other medical emergencies related to dysphagia.
7. Accommodations
Provide accommodations and supportive services as needed, such as extended mealtimes, modified food textures, alternative meal options, or others as suggested by your child’s care team.






