Meltdowns: identifying the triggers and strategies to cope
WHAT CAUSES MELTDOWNS?
There are so many reasons a child could have a meltdown. In my area of work, I most often see meltdowns associated with Sensory Processing Disorder (SPD). For children with this condition, the brain has trouble receiving and processing information from the senses. It leaves many children with anxiety and poor social skills for coping with school and everyday life.
Even if your child is not diagnosed with SPD, a large percentage of routine meltdowns stem from a stimulation overload. Additionally, for children with ADHD, ADD, autism, dyspraxia, or motor coordination problems, sensory processing issues often overlap with their other challenges. This is why understanding how sensory processing works and how any amount of sensory overload can cause meltdowns is critical for parents to understand how to cope and adapt.
WHAT IS SENSORY PROCESSING AND SPD?
If you imagine more than just the five senses, and instead imagine all of the sensations from the environment and our own body that we perceive.
This includes:
• Sight
• Hearing
• Taste
• Smell
• Touch
• Movement
• Body positions
• Internal body process awareness
Here’s an example to illustrate the difference between a person without SPD and a person with. If your hearing informs you that a scene on TV is too loud, then you can easily get up and turn the volume down. Or perhaps the sun is too bright, making it hard to see or to pay attention to what someone is saying because you’re distracted. So, you put on sunglasses and resume normal conversation.
There are many forms of SPD, and each one can affect someone differently. In the above examples, one person with SPD may have an overwhelmed reaction from something much quieter or less obvious as the noisy TV. Another person with SPD may squint and cover her eyes from the bright sun, but not recognise the cause or how to regain stability. She may not be able to carry on the conversation or even keep walking – she is seemingly shut down, standing in the middle of the sidewalk squeezing her head with her hands.
With children, they often can’t recognise, explain or know how to cope with the overwhelmed sensory processing system. This is why an outburst of behaviour – the meltdown – occurs.
MELTDOWN VS TANTRUM
It’s important to understand that a meltdown is not another word for a tantrum. A tantrum is an anger reaction to not getting what one wants. Tantrums are common in all children and often resolve within a few minutes once the parent establishes clear expectations.
Professionals in paediatric behaviour explain a meltdown as an overload of sensations. Despair and total inability to cope are characteristic. Usually the ‘fight or flight’ instinct kicks in, and it can take a long time for a child to be able to resume his activity. Even then, they might be affected for the whole day.
SENSORY THRESHOLDS
A meltdown typically occurs when a situation puts someone past their regulatory sensory threshold.
We all have sensory thresholds – both high and low.
Existing somewhere in the middle is optimal for self-regulation and normal daily functioning, and our typical sensory thresholds fluctuate during the day. If you’re tired, your thresholds might be lower, and you might be irritated easily by noise. If you’re rested and happy, you might enjoy a bit more noise in a social setting.
Someone with SPD has thresholds that are higher and lower than typical (for that culture). A child with a very high threshold might have poor attentions spans, exhibit sensory-seeking behaviours, and limited body awareness.
Conversely, someone whose thresholds are very low might be overly-sensitive, easily overwhelmed, and anxious.
STRATEGIES FOR PARENTS
Here are the techniques I offer parents to cope with their child’s meltdowns.
1. OBSERVE AND BE SENSITIVE TO YOUR CHILD’S SENSORY THRESHOLDS.
Here are some common meltdown triggers to look out for:
- Bright lights/the sun, as evidenced by covering eyes, whining and looking at the ground when walking outside, squinting, looking at the ground and having a hard time sitting still in brightly-lit rooms.
- Loud noises, like traffic sounds, airplanes, construction etc. These are evidenced by covering ears, screaming or crying, shaking, being fearful, hiding behind parents or clutching to their legs.
- Getting dressed/undressed, due to the discomfort or even painful sensation of putting on and taking off clothes. Children will often resist, get angry, cry, lie down and scream and kick or hit to avoid being dressed.
- Crowds, due to the frequency of being touched and bumped by other people. Some children with SPD absolutely hate to be touched, while others are overly-grabby or rough when touching other people.
-
Dining, due to being picky about which textures and temperatures they can eat.
If your child regularly refuses certain categories of foods (crunchy, cold, hot, wet, squishy) then these could be triggers for a meltdown.
2. UNDERSTAND HOW YOUR CHILD REACTS TO APPROACHING HIS SENSORY THRESHOLD.
Observe your child to read the cues that indicate that he’s approaching a sensory threshold. Sometimes a meltdown can be triggered by an obvious event, which you can easily recognise (construction noise for example).
But what about when it seems like there was no trigger at all?
Sometimes, being overwhelmed by choice can trigger a child to shut down. School shopping is a prime example. You’ve asked your child to pick one of several options, over and over from the school supply list. Which backpack: Wolverine or Spiderman? Which colour pencil box? Which lunchbox?
Now your son is tugging at his ears, staring at the ground, and is unresponsive to your queries. You may have not noticed that he was approaching sensory overwhelm.
Or, it could be that your child has a build-up of small triggers throughout the day and then explodes at seemingly nothing. This often happens to children after school. They use up all their energy maintaining calm through the small triggers at school, but when they reach the safety of home, they can’t hold themselves together anymore and ‘go to pieces’.
If you feel like your child has meltdowns out of seemingly nowhere, it’s very likely that you’re dealing with a pattern of escalation of sensory overload. Pay attention to what activities were going on in your child’s life for the few hours leading up his next meltdown. Keeping a journal is a great way to help you notice trends.
3. KNOW WHAT BEHAVIOUR TO EXPECT IN YOUR CHILD WHEN HIS SENSORY THRESHOLD HAS BEEN CROSSED.
What does a full-blown meltdown look like in your child? Does he lie on the ground, screaming and fighting?
Does she cry with wide eyes as if in terror, shaking, and sobbing while clinging to you?
Or is it more of a ‘shut down’, in which your child stops talking, covers his ears or eyes, finds a dark corner to hide in, or tucks his knees to his chest and rocks?
Knowing how your child acts during a meltdown can help you know the right action to take to resolve it.
4. IDENTIFY WHAT WORKS BEST FOR RELIEVING YOUR CHILD FROM A MELTDOWN.
Try out different soothing strategies to see what works best for unwinding your child’s meltdown. Be sure to write them down and give copies to his teachers and other care providers.
Here are some strategies to try:
• Hold your child tightly against you and rock slowly.
• Breathe deeply and slowly while looking into your child’s eyes so she can synchronise her breaths with yours.
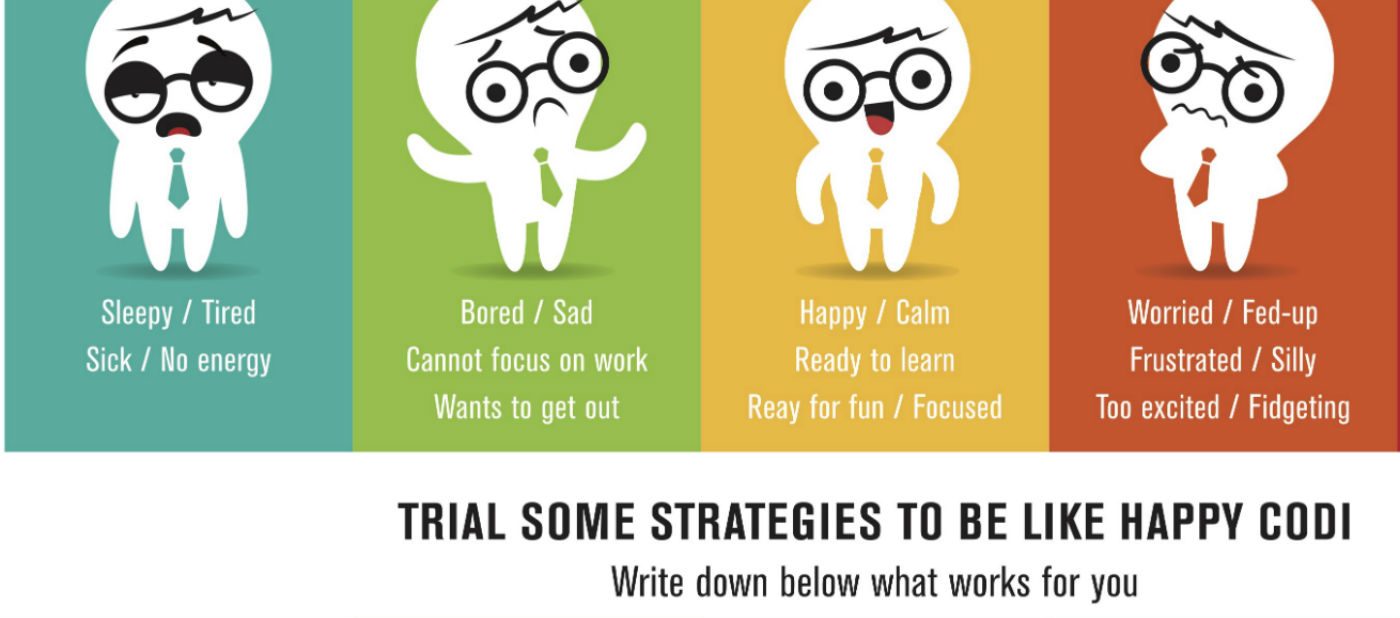
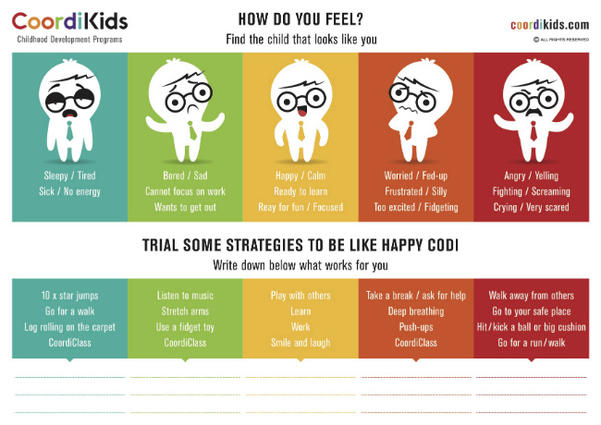
We also use the How Do You Feel chart (below) to help kids to identify how they feel and recognise when a meltdown is building up.
5. A SENSORY DIET
A sensory diet is simply a plan that parents use to ensure that their child receives the sensory-rich activities he seeks at regular intervals throughout the day.
For a child who needs more sensory input, a typical sensory diet would include regular periods of play and movement in an area with high levels of sensory stimulation. He can have 4-5 ‘movement breaks’ in which he can do jumps on the spot, fitness exercises, enjoy a chewy or crunchy snack, carry heavy objects around, or utilise a fidget toy.
For a child with low thresholds who is easily overwhelmed, their sensory diet would include periods of time where she can escape to an environment with very low stimulation. 4-6 times per day, she goes to a quiet, low-lit room where you give a deep- pressure massage with soft music and slow, rhythmic movements for 5 minutes.
I hope that by taking the time to understand some background context for why some children get overwhelmed by certain situations, more parents will be able to set their child up for success in their daily routine. By understanding sensory thresholds and triggers, we can be prepared to diffuse a meltdown before it begins.
Marga Grey (MSc OT) has served as a pediatric occupational therapist for over 40 years with a specialization in sensory integration. She has worked in both private and public settings, including service as a Clinical Educator at Queensland University. Marga developed the occupational therapy department for Tyack Health (the largest multi-disciplinary practice in Australia), where she currently serves as the Leader of the pediatric team. The department, which focuses on pediatric patients, addresses sensory processing and motor skill development. Also, Marga founded the Bayside SPD Professional Interest Group, which educates and raises awareness for Sensory Processing Disorder. As a way to give back to her community, Marga also developed a franchise of day care centres in South Africa to encourage optimal development in young children. Marga regularly provides seminars, workshops and training for therapists and teachers, in person and online through her company CoordiKids. www.CoordiKids.com. Marga is also author of two books, entitled “Sensible Stimulation: The Key to Your Child’s Development During the First Three Years of Life” and “The Sensory Motor Skills: Functional Implications: Stories about fantastic children with sensory motor processing issues.”








